WHAT IS OSTEOPOROSIS?
There was a time when people thought osteoporosis was something that happened to everybody when they got old. Fragile bones and a humped back were inevitable. We now know this is not true. Some people are more likely to get osteoporosis than others. These people have “risk factors” for developing weak and easily broken bones. Many of these risk factors can’t be changed, but others can. Understanding your risks will help you and your healthcare provider takes steps to ensure strong and healthy bones for a lifetime.
Bone Basics
The bony skeleton is an active vital organ. It has two primary functions: structure and storage. Structurally, bones protect your other organs. They create a framework for muscles and tendons that allow you to move. As a storehouse, bones stockpile essential minerals. This ensures they are available when needed. These minerals (mostly calcium) make it possible for the heart to beat; muscles to contract; nerves to conduct impulses; and other bodily processes. We need steady blood levels of calcium at all times. If one system is running short of calcium, the signal goes out requesting more. If there is not enough in circulation, calcium is taken from your bones. This doesn’t cause any harm if happens once in a while. However, too many withdrawals can lead to osteoporosis and bones that break with little if any trauma.
RISK FACTORS THAT CAN’T BE CHANGED
We can’t change the basic biological facts of our lives–things like sex, age, and genetic heritage. Some of these factors are strongly linked with weak bones and osteoporosis. Knowing yours makes it possible to take effective action to protect your bones.
Older Age. People can get osteoporosis at any age, but it is rare under age 50. After middle age, our bones do gradually lose stored reserves of the minerals that make them strong. How fast a person loses bone mineral depends on their health and many other factors. Whatever the cause, when enough mineral is lost, bones break very easily, sometimes without us even knowing it. Some people start out with more bone mineral and lose it more slowly. These people can take a very long time to reach the breaking point, if they reach it at all. On the other hand, the breaking point can come quickly for people who start out with bad health, weak bones, and/or unhealthy eating habits.
Female Gender. Women are twice as likely to get osteoporosis as men. About half of women and one quarter of men over age 50 will break a bone in their remaining lifetime. For women, this is equal to the risk of getting cancers of the breast, ovaries, and uterus combined. For men, the risk is about the same as for getting prostate cancer. Breaking a bone may not sound serious, but it can be. Roughly 20% of people who break a hip die within a year. Another 50% lose their independence and must enter nursing home care.
Menopause. In women, the sex hormone estrogen protects bones through adolescence and young adulthood. When estrogen drops off sharply at menopause, bone mineral loss speeds up, and bones become brittle and more prone to breaking. The problem is worse if a woman goes through menopause early or has her ovaries removed before menopause. In cases like these, bones have both fewer years of estrogen benefits and more years of estrogen loss. This puts the woman at even higher risk for weak bones and fractures.
Family History. Like many things, osteoporosis runs in families. If either of your parents broke a bone as an adult, your risk is higher. Sometimes people don’t even realize they have had a fracture. This is especially true for vertebrae, the small bones in your spine. Vertebrae can break without any symptoms at all. Noticeable height loss and forward bending of the spine may be the first signs that fractures have occurred.
Body Type. Small and thin people tend to break more bones. Many things contribute to this: poor nutrition, low muscle mass, low circulating estrogen, and even less fat “padding” in a fall. If you have very low body weight, your bones don’t have to work very hard to carry you around. If you were heavy, you would have more bone mineral. Starting out with less means any loss makes them weaker, faster. Fortunately, building up muscle and loading up bones through exercise and weight training is proven to help thin, small-boned people improve their bone strength.
Broken Bones/Height Loss. People who break a bone as an adult may already have osteoporosis and not know it. Some broken bones are obvious and some are hard to detect. Vertebral fractures in your spine can be painless. You may feel nothing, but their impact is real. Risk for death goes up 15% in the six months following a vertebral fracture. By slightly changing how weight is balanced on the spine, each broken vertebra raises the risk for another. These fractures may not be discovered until a person has developed extreme curvature of the spine (so-called dowagers hump).
RISK FACTORS THAT CAN BE CHANGED
While our basic biology cannot be changed, many other risk factors for weak bones are within our control. This includes things like nutrition, exercise, and healthy living.
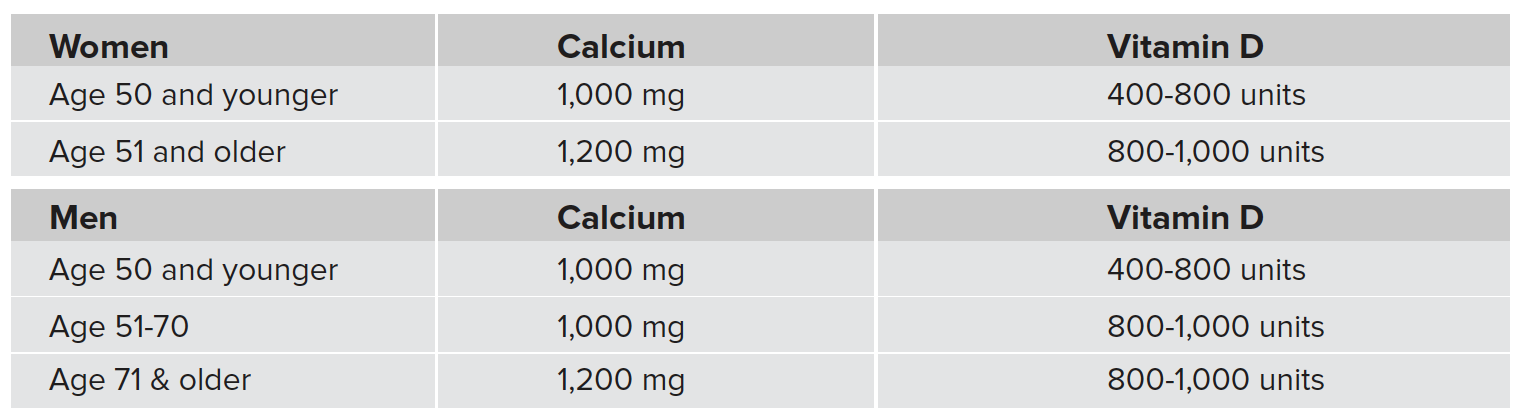
Not Getting Enough Calcium and Vitamin D. Adequate blood calcium drives all our bodily processes. We cannot live without it. Most people can get the calcium they need from foods like cheese, yogurt, leafy greens, and fortified cereals. Calcium tablets are good for filling in when you can’t get enough in your diet, but it is always better to get your calcium from food. Still, calcium by itself is not enough. You also need enough vitamin D. Without vitamin D, your body can’t absorb calcium from the foods you eat. It can be harder to get all the vitamin D you need. Vitamin D is naturally made by bare skin in reaction to sunlight. Many people get too little sun or have skin that doesn’t absorb much vitamin D. This is the case in older adults and darker skinned people. For these individuals, extra effort is needed to avoid bone damage. Because there aren’t many food sources of vitamin D, supplements are recommended for people who need them.
BHOF Recommendations for Daily Calcium and Vitamin D Amounts include all sources, both food and supplements. Get as much of your calcium from food sources as you can.
Not Eating Enough Fruits and Vegetables. We all need to eat fruits and vegetables to have healthy bones. Calcium and vitamin D are only two of the nutrients important for bone. Magnesium, potassium, vitamin K, and others contribute to building and maintaining a strong skeleton. Most experts believe that people can usually get what they need from a balanced diet, rich in fruits and vegetables. Multi-vitamin-mineral supplements are recommended for individuals who have restricted diets, unhealthy eating habits, or digestive problems that interfere with nutrient absorption.
Not Getting Enough Exercise. Bone is a living organ, in a constant process of tearing down and building up. It relies on the push of gravity and the pull of muscle to maintain its strength. Without enough activity, bone mineral and muscle mass are lost at an alarming rate. This is particularly true for people over age 50. The right kind of exercises can help you avoid this. For example, you can do fast walking for weight-bearing and lifting weights for muscle strengthening.
Drinking Too Much. Heavy drinking makes bone weaker and easier to break. By “heavy drinking” we mean more than two alcoholic beverages a day for women or three a day for men. Long-term, it doubles risk for hip fracture in older men. Moderate alcohol intake doesn’t appear to harm bone and may even slightly improve bone strength in postmenopausal women. One drink roughly equals 8-10g of alcohol: 10 oz. beer (285ml), 1.5 oz. liquor (30ml), or 3-4 oz. wine (120ml).
Dieting Too Much. Bones need physical stresses to stay strong. Super-rapid weight reduction causes bone loss by “unloading” the skeleton. Fad diets that scrimp on nutrients, can pull minerals from bones. This leaves them weaker and more likely to break. Safe dieting is slow and steady. Weight loss done right can actually improve bone strength. That is, when it is done along with weight-bearing and resistance exercise, a healthy diet, and plenty of calcium and vitamin D.
Smoking (at all). Most people do not realize that smoking causes skeletal damage and increases the chances they will break a bone. But it does. Taking care of your bones is one of the many reasons to stop tobacco smoking. Broken bones can be disabling. A person’s mobility and independence are at stake. Thinking of it this way may make it easier to stick with a smoking cessation program and quit for good.
MEDICAL CAUSES OF FRAGILE BONES
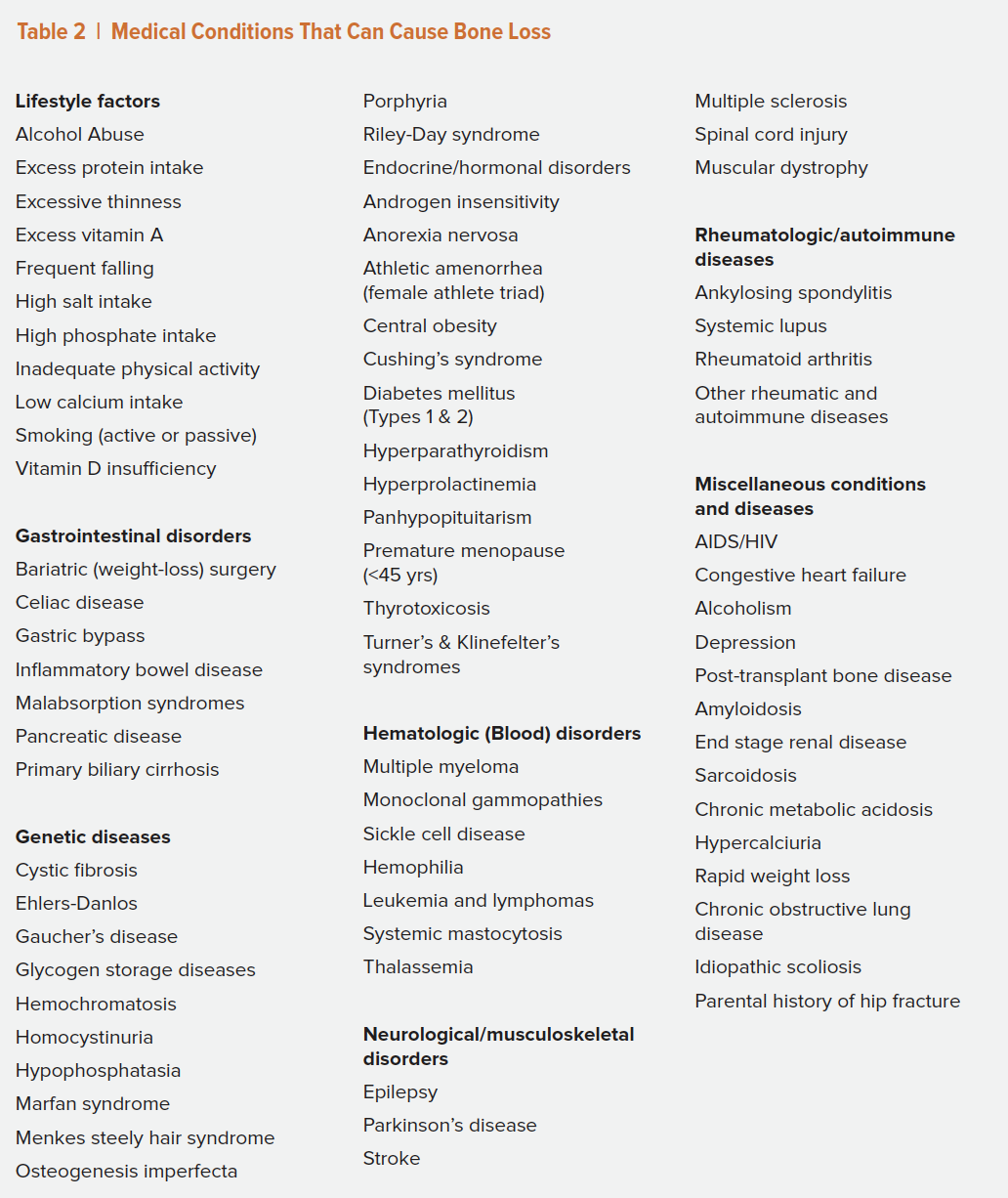
Many health problems can impair calcium metabolism and make your bones more breakable. Damage can be directly caused by a condition, indirectly caused by a condition’s treatment, or caused by a combination of both. Some disorders are linked to bone loss and osteoporosis for reasons not fully understood. One such disorder is depression, which is probably due to multiple factors, some known and some not yet identified.
Below are the some of the many medical causes of bone loss. For a more complete list, see Table 2.
Disorders that Reduce Mobility
Muscles get weak if we don’t use them. Bones are the same. Our bones need stresses that come from moving, lifting, or anything else that works against gravity. Bone suffers when we are inactive, whether due to a disease like multiple sclerosis or to a sedentary lifestyle. Bones also suffer when we are weightless, like astronauts are in space, but this is not likely to be a problem for us. However, at some point in our lives, most of us will be laid up, even if only for a short time.
Stroke, Parkinson’s disease. When you walk, each step transfers impact energy to your skeleton. If you jump, your bones get an even bigger impact. These impacts mobilize bone to add mineral. Without them, bone mineral leaks away, leaving bones weak and breakable. Any condition that restricts the ability to walk causes rapid bone loss, particularly in leg bones that are no longer carrying our weight.
Bed rest following injury/surgery. If you have had surgery anytime in the past few years, you probably noticed that the doctors wanted you up and out of bed as quickly as possible. This is to prevent the bone loss they know will result from bed rest. Calcium absorption goes down; calcium loss goes up. Bones get weaker. The longer the immobilization, the more bone is lost.
Muscle weakness. Bed rest is even worse for your muscles. You can lose 20% of your muscle strength from just one week in bed. Weak muscles lead to weak, more easily broken bones. Smaller muscles exert less push and pull on the bones they are attached to. They can’t share the load when bones get overloaded. They also make it much more likely that if we trip, we will fall. And falls are the number-one cause of broken bones in older adults.
Paralysis. People who use wheelchairs to get around can maintain strength in their arm and back bones through upper-body exercise. Bones in the legs are much harder to preserve without loading. Experimental techniques that use vibration and other passive stresses may prove to be helpful.
Fatigue disorders. Many conditions can cause periods of extreme fatigue. Chronic fatigue syndrome, anemia, sleep apnea, clinical depression, and many other conditions can make a person so tired that they can’t get out of bed. Like muscle, bone responds to exercise by becoming stronger. Without exercise it gets weaker and more likely to break.
Disorders Treated with Glucocorticoid (Steroid) Medications
The immune system is your body’s defender. It produces antibodies to fight off viruses, bacteria, and other “foreign invaders.” Sometimes the immune system goes haywire and can’t tell foreign invaders from normal parts of your body. When this happens, the immune system creates autoantibodies that attack and destroy healthy tissue. This is what is called an autoimmune disease (“auto” means “self”).
Autoimmune diseases are usually treated with steroid medications that calm the immune system. Steroids can control symptoms, but they can also seriously damage bone and cause fractures in the long term.
Inflammatory bowel diseases (IBD). Colitis and Crohn’s disease are common inflammatory bowel diseases (IBDs). Nutrients in food get into the bloodstream through the small intestine, or bowel. When the immune system attacks the bowel, nutrients from food are lost, including calcium and vitamin D needed for healthy bones. Like many other autoimmune diseases, IBDs require steroid treatment, making them doubly bad for bones.
Lupus erythematosus. Lupus is an autoimmune disease that attacks many parts of the body: skin, joints, and/or internal organs. People with lupus have many risk factors for osteoporosis including steroid treatment, inactivity due to pain and fatigue, and the direct action of lupus on bone. To make matters worse, 90% of lupus sufferers are women – already at increased risk for bone loss following menopause.
Organ transplant. Some body parts can be replaced if they stop working. Kidneys, lungs, hearts and other organs can be taken from a donor and transplanted into a sick person. The transplanted organ is “foreign” to the new host’s immune system. To prevent triggering an attack on the transplant, patients must have their immune system shut down temporarily and then held down with steroids for life.
Rheumatoid arthritis. What is usually called “arthritis” is actually osteoarthritis. Osteoarthritis causes sore stiff joints in older people. It is very common and does not cause bone loss. Rheumatoid arthritis (RA) on the other hand, is a serious autoimmune disease that destroys tissue surrounding knees, elbows, and other joints, causing pain, swelling, and disability. On its own, RA increases risk for osteoporosis. When steroids are added to the mix, the risk is even higher.
Sickle cell disease. Sickle cell is a blood disease named for its abnormally (sickle) shaped red blood cells. These defective cells can’t carry oxygen like normal cells and can’t slip easily through tiny blood vessels designed to handle flexible disc-shaped cells. This causes pain, infection, and worse. The most common treatments for adolescents and adults with sickle cell disease are blood transfusions and bone marrow transplants. As with other transplants, steroids are usually needed to prevent immune rejection.
Disorders that Disrupt Nutrient Absorption
Vitamins and minerals are absorbed into the blood stream in the digestive tract (stomach and intestines). Any condition that prevents your body from fully absorbing nutrients from the food you eat is a threat to your bones.
Celiac disease. Celiac disease is an autoimmune disease that causes poor nutrient absorption. Because it can be treated with a gluten-free diet, steroid medications are generally not required. People with celiac disease have trouble digesting gluten found in grains and many prepared foods. This is because their immune system treats gluten as a foreign invader. When gluten is eaten, the body mounts an immune response attacking the small intestine. This greatly reduces absorption of calcium, vitamin D, and other nutrients needed for bone health.
Weight-loss surgery. Operations that remove or close off parts of the stomach and/or intestine can help people lose a lot of weight very quickly. The results are good for general health, but can be bad for bones. There are several reasons for this. First, rapidly unloading your bones makes them lose mineral. Second, food goes through the reduced digestive tract faster and with less-complete absorption. Third, in women, excessive weight loss reduces blood levels of estrogen, which helps maintain healthy bones.
Disorders that Cause Hormone Imbalances
The endocrine system produces hormones that control key functions in the body, everything from blood sugar and muscle strength to bone density. Too much or too little of certain hormones can weaken bones and cause fractures.
Androgen blockers for prostate cancer. Prostate cancer can be fueled by male sex hormones called androgens (mainly testosterone and dihydrotestosterone). Drugs and/or surgeries designed to lower androgen levels are standard treatment for prostate cancer. Men who have had androgen-deprivation therapy can lose bone mass very quickly, sharply raising risk for broken bones.
Diabetes. The hormone insulin keeps blood sugar steady, not too high or too low. The link between insulin and bone health is not completely understood. People with Type 1 (juvenile) diabetes tend to reach adulthood with weak, low-mineral bones that grow more fragile with age. People with Type 2 (“adult onset”) are usually overweight. Although this extra load keeps bone density high, people with Type 2 diabetes break more bones than other people. This may be due to abnormal bone formation, drugs to control blood sugar, and/or side effects of diabetes that make a person more likely to fall. This includes things like vision loss, dizziness, and loss of feeling in the feet.
Eating disorders. The hormone estrogen protects bone. In girls and women, fat-muscle balance has a powerful effect on estrogen levels. When there is too little fat in proportion to muscle, estrogen levels plunge. Eating disorders, such as anorexia nervosa, harm bones by reducing estrogen and by robbing the body of needed nutrients. Although less common in men, eating disorders cause bone loss in males as well.
Estrogen blockers for breast cancer. Fragile bones and fractures are much more common in women who have been treated for breast cancer. Certain types of breast cancer are worsened by estrogen. Treatment involves reducing estrogen with drugs like tamoxifen and aromatase inhibitors. Anti-estrogen drugs are often given in combination with chemotherapy–which can damage ovaries and induce early menopause.
Low male sex hormones (androgens). Male bone is protected by androgens. Gradual decline in these hormones is a normal part of aging. However, if levels get too low, bone loss and fractures can follow. Besides aging, low androgens in men can result from alcoholic drinking, eating disorders, obesity, kidney disease, and many other health problems. If a man’s blood test shows low androgens, his doctor will most likely want to follow up with additional tests.
Missed or irregular periods. In young women, having an irregular menstrual cycle can be symptom of problems with estrogen or pituitary hormones. Both of these hormones are essential to growing and maintaining strong bones. Any woman with missed or irregular periods should check in with her gynecologist or primary care doctor.
Abnormal levels of parathyroid hormone. Parathyroid hormone controls how much calcium circulates in the blood stream. This is very important to bones. Too much parathyroid hormone reduces calcium in circulation, depriving bones of needed building material. Vitamin D deficiency triggers excess production of parathyroid hormone. Usually restoring healthy blood levels of vitamin D will correct calcium imbalance and may even rebuild some of the lost bone.
Abnormal levels of thyroid hormone. Thyroid hormone controls how fast your body uses energy. You could say it controls the speed of your body’s motor. Too little and the motor slows down, too much and it speeds up. The effect on bones depends on your age and other factors. In childhood, too little thyroid hormone (hypothyroidism) impairs growth and skeletal development. In adulthood, too much (hyperthyroidism) weakens muscles and leaves bones fragile and easy to break.
There are many other illnesses and medical conditions that increase risk for bone loss and fractures. Table 2 lists many of them, including activity and dietary habits, genetic conditions, and progressive diseases. You can’t change your basic biology but you can make healthy choices that preserve your bones. Although it is not always possible to cure an illness, it may be possible to successfully manage it without harming your bones in the process.
Medicines that May Cause Bone Loss
Many medications can cause loss of bone mineral that leads to osteoporosis and fractures. We have talked already about two of the worst offenders: steroids and sex-hormone blockers.
The drugs listed here are used to treat serious illness. When needed, their benefits usually far outweigh their risks. You would never want to stop taking something prescribed without discussing it with your healthcare provider. Alternate drugs may be available; lower doses or shorter courses might work equally well. Do not experiment on your own. Talk with your doctor before making any changes.
If you take any drugs on this list or have any of the medical conditions we talked about earlier, ask your healthcare provider about steps you can take to prevent osteoporosis. Together, you can develop a plan to protect your bones for a lifetime.
For additional information, visit the Bone Health & Osteoporosis Foundation (BHOF) website at bonehealthandosteoporosis.org. There you will find newsletters, handbooks on exercise and safe movement, ant-fracture medications, access to support groups, and more.